Extracellular xenogeneic hemoglobin suppresses the capacity for C2C12 myoblast myogenic differentiation
Keywords:
extracellular hemoglobin, C2C12 cells, myogenic differentiation, proliferation, migrationAbstract
Paper description:
- As a part of their microenvironment, extracellular hemoglobin has the potential to modify functional characteristics of satellite cells that act as myogenesis initiators.
- The effect of extracellular xenogeneic hemoglobin (porcine and bovine) was investigated on myoblast proliferation, migration and differentiation capacity, using C2C12 cells as a model.
- Extracellular hemoglobin modifies C2C12 cell proliferation and migration in a dose- and time-dependent manner and suppresses myogenic differentiation.
- These findings are important for treating muscle injuries in patients with hemoglobinemia-related diseases and conditions, especially when using satellite cells for cell therapy as the presence of extracellular hemoglobin can influence its outcome.
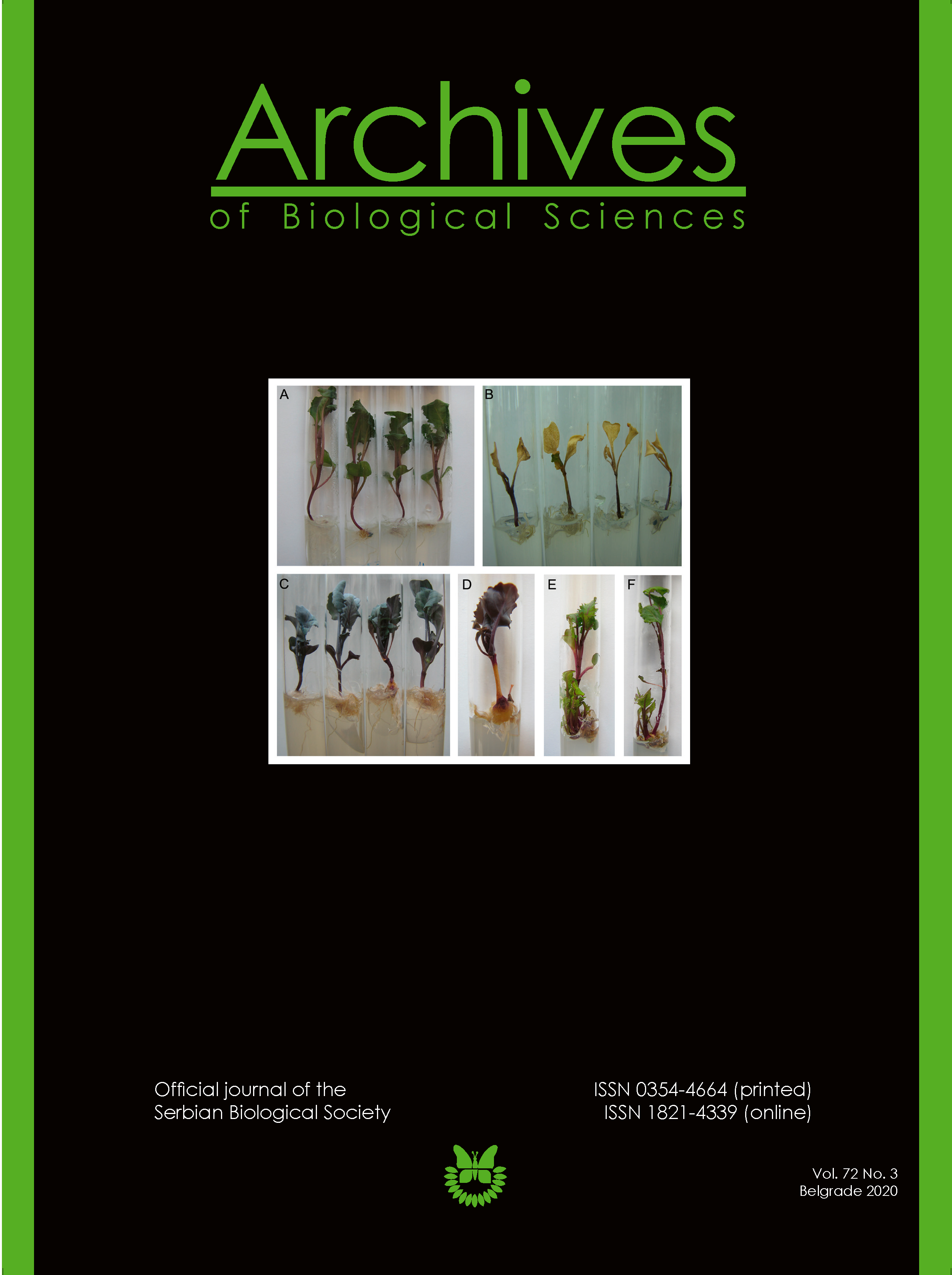
Abstract: Functional characteristics of satellite cells (SCs) that act as myogenesis initiators and have emerged as a promising target for cell therapy, are dependent on their microenvironment. The aim of this study was to investigate the effect of cell-free hemoglobin, as a part of the microenvironment of SCs, on their functional characteristics. The C2C12 cell line served as the experimental model of the SC experimental model; hemoglobin isolated from porcine (PHb) and bovine (BHb) slaughterhouse blood served as the extracellular hemoglobin. The proliferation rate of C2C12 cells was assessed by the MTT test, migration capacity by the scratch assay, and myogenic differentiation capacity by histochemical staining and RT-PCR analysis of the expression of genes specific for myogenic lineage. The effect of hemoglobin on the proliferation and migration of C2C12 cells was dependent on its concentration and the animal species it was isolated from, but the effect of BHb was more prominent. Both PHb and BHb decreased the expression levels of myogenin and muscle specific creatine kinase at a 10 µM concentration. While PHb had no effect on the morphometric parameters of C2C12 myotubes, BHb modified the area and length of C2C12 myotubes cultivated in DMEM/2% horse serum and DMEM/10% fetal calf serum. While PHb and BHb had no effect on heme oxygenase 1 (Hmox1) expression, they stimulated the expression of hypoxia-inducible factor 1-alpha (Hif1α) at a concentration of 10 µM. The mainly inhibitory effect of cell-free hemoglobin on myogenic differentiation suggests that it could be a relevant factor in the outcome of cell therapy of muscle injury.
https://doi.org/10.2298/ABS200625032S
Received: June 25, 2020; Revised: August 8, 2020; Accepted: August 10, 2020; Published online: August 25, 2020
How to cite this article: Stančić AZ, Drvenica IT, Bugarski BM, Ilić VL, Bugarski DS. Extracellular xenogeneic hemoglobin suppresses the capacity for C2C12 myoblast myogenic differentiation. Arch Biol Sci. 2020;72(3):379-91.
Downloads
References
Järvinen TAH, Järvinen TLN, Kääriäinen M, Äärimaa V, Vaittinen S, Kalimo H, Järvinen M. Muscle injuries: optimising recovery. Best Pract Res Clin Rheumatol. 2007;21(2):317-31.
Qazi TH, Duda GN, Ort MJ, Perka C, Geissler S, Winkler T. Cell therapy to improve regeneration of skeletal muscle injuries. J Cachexia Sarcopenia Muscle. 2019;10:501-16.
Chiu CH, Chang TH, Chang SS, Chang GJ, Chen ACY, Cheng CY, Chen SC, Fu JF, Wen CJ, Chan YS. Application of bone marrow-derived mesenchymal stem cells for muscle healing after contusion injury in mice. Am J Sports Med. 2020;48(5):1226-35.
Liu Z, Mikrani R, Zubair HM, Taleb A, Naveed M, Baig MMFA, Zhang Q, Li C, Habib M, Cui X, Sembatya KR, Lei H, Xiaohui Z. Systemic and local delivery of mesenchymal stem cells for heart renovation: Challenges and innovations. Eur J Pharmacol. 2020;876:173049.
Toumi H, Best TM. The inflammatory response: Friend or enemy for muscle injury? Br J Sports Med. 2003;37(4):284-6.
Yin H, Price F, Rudnicki MA. Satellite cells and the muscle stem cell niche. Physiol Rev. 2013;93(1):23-67.
Tierney MT, Sacco A. Satellite cell heterogeneity in skeletal muscle homeostasis. Trends Cell Biol. 2016;26(6):434-44.
Fujita H, Endo A, Shimizu K, Nagamori E. Evaluation of serum-free differentiation conditions for C2C12 myoblast cells assessed as to active tension generation capability. Biotechnol Bioeng. 2010;107(5):894-901.
Mallet V, Dutheil D, Polard V, Rousselot M, Leize E, Hauet T, Goujon JM, Zal F. Dose-ranging study of the performance of the natural oxygen transporter HEMO2life in organ preservation. Artif Organs. 2014;38(8):691-701.
Zal F, Rousselot M. Extracellular hemoglobins from annelids, and their potential use in biotechnology. In: La Barre S, Kornprobst JM, editors. Outstanding Marine Molecules: Chemistry, Biology, Analysis. Hoboken: Wiley-Blackwell; 2014. p. 361-76.
Le Pape F, Gaëlle R, Porchet E, Sourice S, Dubrana F, Férec C, Polard V, Pace R, Weiss P, Zal F, Delépine P, Leize E. Adhesion, proliferation and osteogenic differentiation of human MSCs cultured under perfusion with a marine oxygen carrier on an allogenic bone substitute. Artif Cells Nanomed Biotechnol. 2017;46(1):95-107.
Stančić AZ, Drvenica IT, Obradović HN, Bugarski BM, Lj Ilić V, Bugarski DS. Native bovine hemoglobin reduces differentiation capacity of mesenchymal stromal cells in vitro. Int J Biol Macromol. 2020;144:909-20.
Yang Q, Bai S-Y, Li L-F, Li S, Zhang Y, Munir M, Qiu HJ. Human hemoglobin subunit beta functions as a pleiotropic regulator of the RIG-I/MDA5-mediated antiviral innate immune responses. J Virol. 2019;93(16). e00718-19.
Wang Y, Wang L, Yu W, Gao D, You G, Li P, Zhang S, Zhang J, Hu T, Zhao L, Zhou H. A PEGylated bovine hemoglobin as a potent hemoglobin-based oxygen carrier. Biotechnol Prog. 2017;33(1):252-60.
Kostić IT, Ilić VL, Đorđević VB, Bukara KM, Mojsilović SB, Nedović VA, Bugarski DS, Veljović ĐN, Mišić DM, Bugarski BM. Erythrocyte membranes from slaughterhouse blood as potential drug vehicles: Isolation by gradual hypotonic hemolysis and biochemical and morphological characterization. Colloids Surf B. 2014;122:250-9.
Drvenica IT, Stančić AZ, Kalušević A, Marković S, Dragišić Maksimović J, Nedović VA, Bugarski BM, Ilić VLj. Maltose-mediated long-term stabilization of freeze- and spray-dried forms of bovine and porcine hemoglobin. J Serbian Chem Soc. 2019; 84(10):1105-17.
Veselinovic M, Vasiljevic D, Vucic V, Arsic A, Petrovic S, Tomic-Lucic A, Savic M, Zivanovic S, Stojic V, Jakovljevic V. Clinical benefits of n-3 PUFA and ɤ-linolenic acid in patients with rheumatoid arthritis. Nutrients. 2017;9(4):325-35.
Folch J, Less M, Sloane Stanley G. A simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem. 1957;226(1):497-509.
Gloster J, Fletcher R. Quantitative analysis of serum lipids with thin-layer chromatography. Clin Chim Acta. 1966;13(2):235-240.
Ristic-Medic D, Suzic S, Vucic V, Takic M, Tepsic J, Glibetic M. Serum and erythrocyte membrane phospholipids fatty acid composition in hyperlipidemia: Effects of dietary intervention and combined diet and fibrate therapy. Gen Physiol Biophys. 2009;28:190- 9.21.Mosmann T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J Immunol Methods. 1983;65(1-2):55-63.
Kocić J, Santibañez JF, Krstić A, Mojsilović S, Đorđević IO, Trivanović D, Ilić V, Bugarski D. Interleukin 17 inhibits myogenic and promotes osteogenic differentiation of C2C12 myoblasts by activating ERK1,2. Biochim Biophys Acta - Mol Cell Res. 2012;1823(4):838-49.
Yeh TS, Hsu CC, Yang SC, Hsu MC, Liu JF. Angelica Sinensis promotes myotube hypertrophy through the PI3K/Akt/mTOR pathway. BMC Complement Altern Med. 2014;14:1-9.
Quaye IK. Extracellular hemoglobin: The case of a friend turned foe. Front Physiol. 2015;6(96):1-13.
Schaer DJ, Buehler PW, Alayash AI, Belcher JD, Vercellotti GM. Hemolysis and free hemoglobin revisited: exploring hemoglobin and hemin scavengers as a novel class of therapeutic proteins. Blood. 2013;121(8):1276-85.
Jeney V. Pro-inflammatory actions of red blood cell-derived DAMPs. Exp Suppl. 2018;108:211-33.
Ferrer I, Gómez A, Carmona M, Huesa G, Porta S, Riera-Codina M, Biagioli M, Gustincich S, Aso E. Neuronal hemoglobin is reduced in Alzheimer’s disease, argyrophilic grain disease, Parkinson’s disease, and Dementia with Lewy bodies. J Alzheimers Dis. 2011;23(3):537-50.
Bamm V V., Henein MEL, Sproul SLJ, Lanthier DK, Harauz G. Potential role of ferric hemoglobin in MS pathogenesis: Effects of oxidative stress and extracellular methemoglobin or its degradation products on myelin components. Free Radic Biol Med. 2017;112:494-503.
Erdei J, Tóth A, Nagy A, Nyakundi BB, Fejes Z, Nagy B, Novák L, Bognár L, Balogh E, Paragh G, Kappelmayer J, Bácsi A, Jeney V. The role of hemoglobin oxidation products in triggering inflammatory response upon intraventricular hemorrhage in premature infants. Front Immunol. 2020;11:228-41.
Bellos I, Pergialiotis V, Loutradis D, Papapanagiotou A, Daskalakis G. The role of hemoglobin degradation pathway in preeclampsia: A systematic review and meta-analysis. Placenta. 2020;92:9-16.
Klimczak A, Kozlowska U, Kurpisz M. Muscle stem/progenitor cells and mesenchymal stem cells of bone marrow origin for skeletal muscle regeneration in muscular dystrophies. Arch Immunol Ther Exp (Warsz). 2018;66(5):341-54.
Li Y, Fan Y, Pan H, Qian H, Qi X, Wu G, Zhang H, Xu M, Rao Z, Wang L, Ying H. Effects of functional β-glucan on proliferation, differentiation, metabolism and its anti-fibrosis properties in muscle cells. Int J Biol Macromol. 2018;117:287-93.
Kristiansen M, Graversen JH, Jacobsen C, Sonne O, Hoffman HJ, Law SKA, Moestrup SK. Identification of the haemoglobin scavenger receptor. Nature. 2001;409(6817):198-201.
Ferguson SK, Harral JW, Pak DI, Redinius KM, Stenmark KR, Schaer DJ, Buehler PW, Irwin DC. Impact of cell-free hemoglobin on contracting skeletal muscle microvascular oxygen pressure dynamics. Nitric Oxide. 2018;76:29-36.
Le Pape F, Cosnuau-Kemmat L, Gaëlle R, Dubrana F, Férec C, Zal F, Leize E, Delépine P. HEMOXCell, a new oxygen carrier usable as an additive for mesenchymal stem cell culture in platelet lysate-supplemented media. Artif Organs. 2017;41(4):359-71.
Le Pape F, Bossard M, Dutheil D, Rousselot M, Polard V, Férec C, Leize E, Delépine P, Zal F. Advancement in recombinant protein production using a marine oxygen carrier to enhance oxygen transfer in a CHO-S cell line. Artif Cells Nanomed Biotechnol. 2015;43(3):186-95.
Wang Y, Zhang T, Zhang H, Yang H, Li Y, Jiang Y. Bovine hemoglobin derived peptide Asn-Phe-Gly-Lys inhibits pancreatic cancer cells metastasis by targeting secreted Hsp90α. J Food Sci. 2017;82(12):3005-12.
Fischer-Fodor E, Mot A, Deac F, Arkosi M, Silaghi-Dumitrescu R. Towards hemerythrin-based blood substitutes: Comparative performance to hemoglobin on human leukocytes and umbilical vein endothelial cells. J Biosci. 2011;36(2):215-21.
Roth AD, Elmer J, Harris DR, Huntley J, Palmer AF, Nelson T, Johnson JK, Xue R, Lannutti JJ, Viapiano MS. Hemoglobin regulates the migration of glioma cells along poly(ε-caprolactone)-aligned nanofibers. Biotechnol Prog. 2014;30(5):1214-20.
Yang Y, Xi Z, Xue Y, Ren J, Sun Y, Wang B, Zhong Z, Yang G, Sun Q, Bian L. Hemoglobin pretreatment endows rat cortical astrocytes resistance to hemin-induced toxicity via Nrf2/HO-1 pathway. Exp Cell Res. 2017;361(2):217-24.
Lara FA, Kahn SA, Da Fonseca ACC, Bahia CP, Pinho JPC, Graca-Souza AV, Houzel JC, de Oliveira PL, Moura-Neto V, Oliveira MF. On the fate of extracellular hemoglobin and heme in brain. J Cereb Blood Flow Metab. 2009;29(6):1109-20.
Ortegon DP, Davis MR, Dixon PS, Smith DL, Josephs JD, Mueller DL, Jenkins DH, Kerby JD. The polymerized bovine hemoglobin-based oxygen-carrying solution (HBOC-201) is not toxic to neural cells in culture. J Trauma. 2002;53(6):1068-72.
Lee RA, Kim HA, Kang BY, Kim KH. Hemoglobin induces colon cancer cell proliferation by release of reactive oxygen species. World J Gastroenterol. 2006;12(35):5644-50.
Chen G, Palmer AF. Hemoglobin regulates the metabolic, synthetic, detoxification, and biotransformation functions of hepatoma cells cultured in a hollow fiber bioreactor. Tissue Eng Part A. 2010;16(10):3231-40.
Yang Y, Ren J, Sun Y, Xue Y, Zhang Z, Gong A, Wang B, Zhong Z, Cui Z, Xi Z, Yang G, Sun Q, Bian L. A connexin43/YAP axis regulates astroglial-mesenchymal transition in hemoglobin induced astrocyte activation. Cell Death Differ. 2018;25(10):1870-84.
Pagliacci MC, Spinozzi F, Migliorati G, Fumi G, Smacchia M, Grignani F, Riccardi C, Nicoletti I. Genistein inhibits tumour cell growth in vitro but enhances mitochondrial reduction of tetrazolium salts: A further pitfall in the use of the MTT assay for evaluating cell growth and survival. Eur J Cancer. 1993;29(11):1573-7.
Gordon J, Brown M, Reynolds M. Cell-based methods for determination of efficacy for candidate therapeutics in the clinical management of cancer. Diseases. 2018;6(4):85.
Bo J, Guan Y, Guo Y, Xie S, Zhang C, Zhang H, Chen Z, Lu J, Meng QH. Impairment of endothelial cell function induced by hemoglobin A1c and the potential mechanisms. Exp Clin Endocrinol Diabetes. 2015;123(9):529-35.
Veliça P, Bunce CM. A quick, simple and unbiased method to quantify C2C12 myogenic differentiation. Muscle Nerve. 2011;44(3):366-70.
Baird MF, Graham SM, Baker JS, Bickerstaff GF. Creatine-kinase- and exercise-related muscle damage implications for muscle performance and recovery. J Nutr Metab. 2012;2012:960363.
Van Deursen J, Ruitenbeek W, Heerschap A, Jap P, Ter Laak H, Wieringa B. Creatine kinase (CK) in skeletal muscle energy metabolism: A study of mouse mutants with graded reduction in muscle CK expression. Proc Natl Acad Sci U S A. 1994;91(19):9091-5.
Funanage VL, Schroedl NA, Moses PA, Smith SM, Kirwin JJ, Hartzell CR. Hemin enhances differentiation and maturation of cultured regenerated skeletal myotubes. J Cell Physiol. 1989;141(3):591-7.
Gustafsson M V., Zheng X, Pereira T, Gradin K, Jin S, Lundkvist J, Ruas JL, Poellinger L, Lendahl U, Bondesson M. Hypoxia requires Notch signaling to maintain the undifferentiated cell state. Dev Cell. 2005;9(5):617-28.
Guo Y, Chi X, Wang Y, Heng BC, Wei Y, Zhang X, Zhao H, Yin Y, Deng X. Mitochondria transfer enhances proliferation, migration, and osteogenic differentiation of bone marrow mesenchymal stem cell and promotes bone defect healing. Stem Cell Res Ther. 2020;11(1):245.
Gordon J, Brown M, Reynolds M. Cell-based methods for determination of efficacy for candidate therapeutics in the clinical management of cancer. Diseases. 2018; 6(4):85.
Wang F, Zhu L, Chen X, Liu G, Fan M. [Hypoxia enhances the proliferation of skeletal myoblasts and possible mechanism]. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2010;26(2):133-6. Chinese.
Hardison RC. Evolution of hemoglobin and its genes. Cold Spring Harb Perspect Med. 2012;2(12):1-18.
Gaudry MJ, Storz JF, Butts GT, Campbell KL, Hoffmann FG. Repeated evolution of chimeric fusion genes in the β-globin gene family of laurasiatherian mammals. Genome Biol Evol. 2014;6(5):1219-33.
Abreu P, Pinheiro CHJ, Vitzel KF, Vasconcelos DAA, Torres RP, Fortes MS, Marzuca-Nassr GN, Mancini-Filho J, Hirabara SM, Curi R. Contractile function recovery in severely injured gastrocnemius muscle of rats treated with either oleic or linoleic acid. Exp Physiol. 2016;101(11):1392-405.
He L, Tian X, Yan C, Liu D, Wang S, Han Y. Nicotine promotes the differentiation of C2C12 myoblasts and improves skeletal muscle regeneration in obese mice. Biochem Biophys Res Commun. 2019;511(4):739-45.
Yayoi T, Kawaharada R, Ishida C, Nakamura A. Effects of saturated fatty acids on skeletal muscle differentiation in an intrauterine hyperglycemic environment. Proc Annu Meet Japanese Pharmacol Soc. 2020;93(0):1-P-079.
Magee P, Pearson S, Allen J. The omega-3 fatty acid, eicosapentaenoic acid (EPA), prevents the damaging effects of tumour necrosis factor (TNF)-alpha during murine skeletal muscle cell differentiation. Lipids Health Dis. 2008;7:1-11.
Peng Y, Zheng Y, Zhang Y, Zhao J, Chang F, Lu T, Zhang R, Li Q, Hu X, Li N. Different effects of omega-3 fatty acids on the cell cycle in C2C12 myoblast proliferation. Mol Cell Biochem. 2012;367(1-2):165-73.
Stoll LL, Spector AA. Changes in serum influence the fatty acid composition of established cell lines. In Vitro. 1984;20(9):732-8.
Bhullar AS, Putman CT, Mazurak VC. Potential role of omega-3 fatty acids on the myogenic program of satellite cells. Nutr Metab Insights. 2016;9:1-10.
Downloads
Published
How to Cite
Issue
Section
License
Authors grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution 4.0 International License that allows others to share the work with an acknowledgment of the work’s authorship and initial publication in this journal.